Celiac disease (gluten-sensitive enteropathy), sometimes called sprue or coeliac, is an immune reaction to eating gluten, a protein found in wheat, barley and rye.
If you have celiac disease, eating gluten triggers an immune response in your small intestine. Over time, this reaction damages your small intestine's lining and prevents absorption of some nutrients (malabsorption). The intestinal damage often causes diarrhea, fatigue, weight loss, bloating and anemia, and can lead to serious complications.
In children, malabsorption can affect growth and development, in addition to the symptoms seen in adults.
There's no cure for celiac disease — but for most people, following a strict gluten-free diet can help manage symptoms and promote intestinal healing.
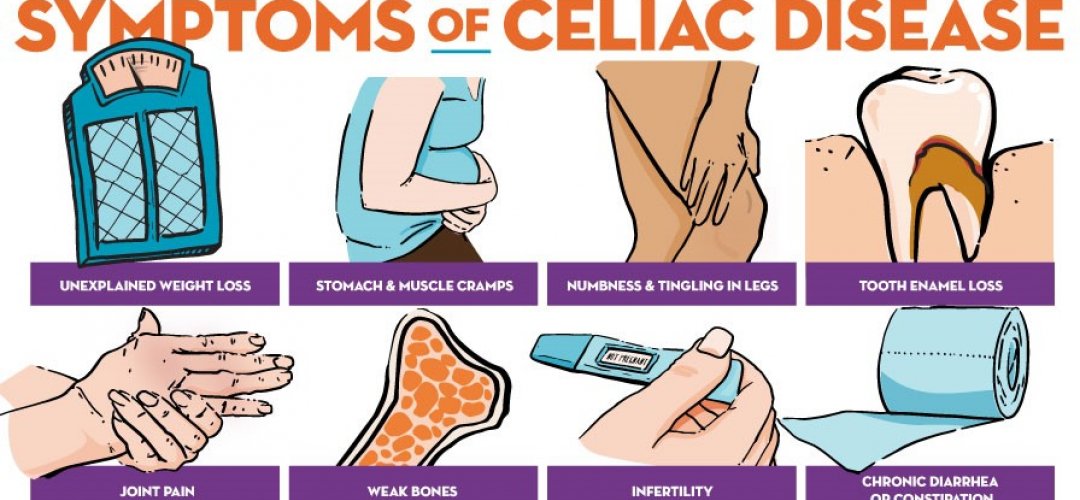
Symptoms
The signs and symptoms of celiac disease can vary greatly and are different in children and adults. The most common signs for adults are diarrhea, fatigue and weight loss. Adults may also experience bloating and gas, abdominal pain, nausea, constipation, and vomiting.
However, more than half of adults with celiac disease have signs and symptoms that are not related to the digestive system, including:
- Anemia, usually resulting from iron deficiency
- Loss of bone density (osteoporosis) or softening of bone (osteomalacia)
- Itchy, blistery skin rash (dermatitis herpetiformis)
- Damage to dental enamel
- Mouth ulcers
- Headaches and fatigue
- Nervous system injury, including numbness and tingling in the feet and hands, possible problems with balance, and cognitive impairment
- Joint pain
- Reduced functioning of the spleen (hyposplenism)
- Acid reflux and heartburn
Children
In children under 2 years old, typical signs and symptoms of celiac disease include:
- Vomiting
- Chronic diarrhea
- Swollen belly
- Failure to thrive
- Poor appetite
- Muscle wasting
Older children may experience:
- Diarrhea
- Constipation
- Weight loss
- Irritability
- Short stature
- Delayed puberty
- Neurological symptoms, including attention-deficit/hyperactivity disorder (ADHD), learning disabilities, headaches, lack of muscle coordination and seizures
Dermatitis herpetiformis
Dermatitis herpetiformis is an itchy, blistering skin disease that stems from intestinal gluten intolerance. The rash usually occurs on the elbows, knees, torso, scalp and buttocks.
Dermatitis herpetiformis is often associated with changes to the lining of the small intestine identical to those of celiac disease, but the disease may not produce noticeable digestive symptoms.
Doctors treat dermatitis herpetiformis with a gluten-free diet or medication, or both, to control the rash.
When to see a doctor
Consult your doctor if you have diarrhea or digestive discomfort that lasts for more than two weeks. Consult your child's doctor if your child is pale, irritable or failing to grow or has a potbelly and foul-smelling, bulky stools.
Be sure to consult your doctor before trying a gluten-free diet. If you stop or even reduce the amount of gluten you eat before you're tested for celiac disease, you may change the test results.
Celiac disease tends to run in families. If someone in your family has the condition, ask your doctor if you should be tested. Also ask your doctor about testing if you or someone in your family has a risk factor for celiac disease, such as type 1 diabetes.
Causes
Celiac disease occurs from an interaction between genes, eating foods with gluten and other environmental factors, but the precise cause isn't known. Infant feeding practices, gastrointestinal infections and gut bacteria might contribute to developing celiac disease.
Sometimes celiac disease is triggered — or becomes active for the first time — after surgery, pregnancy, childbirth, viral infection or severe emotional stress.
When the body's immune system overreacts to gluten in food, the reaction damages the tiny, hair-like projections (villi) that line the small intestine. Villi absorb vitamins, minerals and other nutrients from the food you eat. If your villi are damaged, you can't get enough nutrients, no matter how much you eat.
Some gene variations appear to increase the risk of developing the disease. But having those gene variants doesn't mean you'll get celiac disease, which suggests that additional factors must be involved.
The rate of celiac disease in Western countries is estimated at about 1 percent of the population. Celiac disease is most common in Caucasians; however, it is now being diagnosed among many ethnic groups and is being found globally.
Risk factors
Celiac disease can affect anyone. However, it tends to be more common in people who have:
- A family member with celiac disease or dermatitis herpetiformis
- Type 1 diabetes
- Down syndrome or Turner syndrome
- Autoimmune thyroid disease
- Microscopic colitis (lymphocytic or collagenous colitis)
- Addison's disease
- Rheumatoid arthritis
Complications
Untreated, celiac disease can cause:
- Malnutrition. The damage to your small intestine means it can't absorb enough nutrients. Malnutrition can lead to anemia and weight loss. In children, malnutrition can cause slow growth and short stature.
- Loss of calcium and bone density. Malabsorption of calcium and vitamin D may lead to a softening of the bone (osteomalacia or rickets) in children and a loss of bone density (osteoporosis) in adults.
- Infertility and miscarriage. Malabsorption of calcium and vitamin D can contribute to reproductive issues.
- Lactose intolerance. Damage to your small intestine may cause you to experience abdominal pain and diarrhea after eating lactose-containing dairy products, even though they don't contain gluten. Once your intestine has healed, you may be able to tolerate dairy products again. However, some people continue to experience lactose intolerance despite successful management of celiac disease.
- Cancer. People with celiac disease who don't maintain a gluten-free diet have a greater risk of developing several forms of cancer, including intestinal lymphoma and small bowel cancer.
- Neurological problems. Some people with celiac disease may develop neurological problems such as seizures or peripheral neuropathy (disease of the nerves that lead to the hands and feet).
In children, celiac disease can also lead to failure to thrive, delayed puberty, weight loss, irritability and dental enamel defects, anemia, arthritis, and epilepsy.
Nonresponsive celiac disease
As many as 30 percent of people with celiac disease may not have, or be able to maintain, a good response to a gluten-free diet. This condition, known as nonresponsive celiac disease, is often due to contamination of the diet with gluten. Therefore it's important to work with a dietitian.
People with nonresponsive celiac disease may have additional conditions, such as bacteria in the small intestine (bacterial overgrowth), microscopic colitis, poor pancreas function, irritable bowel syndrome or intolerance to disaccharides (lactose and fructose). Or, they may have refractory celiac disease.
Refractory celiac disease
In rare instances, the intestinal injury of celiac disease persists and leads to substantial malabsorption, even though you have followed a strict gluten-free diet. This combination is known as refractory celiac disease.
If you continue to experience signs and symptoms despite following a gluten-free diet for six months to one year, your doctor may recommend further testing and look for other explanations for your symptoms. Your doctor may recommend treatment with a steroid to reduce intestinal inflammation, or a medication that suppresses your immune system. All patients with celiac disease should be followed up to monitor the response of their disease to treatment.
Diagnosis
Researchers estimate that only 20 percent of people with celiac disease may receive a diagnosis.
Doctors may order two blood tests to help diagnose celiac disease.
- Serology testing looks for antibodies in your blood. Elevated levels of certain antibody proteins indicate an immune reaction to gluten.
- Genetic testing for human leukocyte antigens (HLA-DQ2 and HLA-DQ8) can be used to rule out celiac disease.
If the results of these tests indicate celiac disease, your doctor may order an endoscopy to view your small intestine and to take a small tissue sample (biopsy) to analyze for damage to the villi.
It's important to be tested for celiac disease before trying a gluten-free diet. Eliminating gluten from your diet may change the results of blood tests so that they appear to be normal.
Treatment
A strict, lifelong gluten-free diet is the only way to manage celiac disease. In addition to wheat, foods that contain gluten include:
- Barley
- Bulgur
- Durum
- Farina
- Graham flour
- Malt
- Rye
- Semolina
- Spelt (a form of wheat)
- Triticale
Your doctor may refer you to a dietitian, who can help you plan a healthy gluten-free diet.
Once you remove gluten from your diet, inflammation in your small intestine generally begins to lessen — usually within several weeks, though you may start to feel better in just a few days. Complete healing and regrowth of the villi may take several months to several years. Healing in the small intestine tends to occur more quickly in children than adults.
If you accidentally eat a product that contains gluten, you may experience abdominal pain and diarrhea. Some people experience no signs or symptoms after eating gluten, but this doesn't mean it's not harmful to them. Even trace amounts of gluten in your diet can be damaging, whether or not they cause signs or symptoms.
Hidden gluten can be present in foods, medications and nonfood products, including:
- Modified food starch, preservatives and food stabilizers
- Prescription and over-the-counter medications
- Vitamin and mineral supplements
- Herbal and nutritional supplements
- Lipstick products
- Toothpaste and mouthwash
- Envelope and stamp glue
- Play-Doh
Vitamin and mineral supplements
If your nutritional deficiencies are severe, your doctor or dietitian may recommend taking vitamin and mineral supplements. You may need to supplement your levels of:
- Calcium
- Folate
- Iron
- Vitamin B-12
- Vitamin D
- Vitamin K
- Zinc
Vitamins and supplements are usually taken in pill form. If your digestive tract has trouble absorbing vitamins, your doctor may give them by injection. You need to be sure that the vitamins and supplements are gluten-free.
Follow-up care
If you have celiac disease, you will need medical follow-up to make sure your symptoms have responded to a gluten-free diet. Doctors will also want to be sure you are getting the support you need to maintain the diet for life. They will use blood tests to monitor your response. The results of these tests, which are primarily designed as a way to detect celiac disease, usually become negative once you have been gluten-free for six to 12 months. If test results remain positive, then your doctor may try to find the reason, the most common being unintentional exposure to gluten in your diet.
However, these tests are not perfect, and even if the results become negative, it is possible that you could still be exposed to a significant amount of gluten and continue to have symptoms and damage to your intestines.
If you continue to have symptoms, or your symptoms recur, you may need a follow-up endoscopy with biopsies to ensure that healing has occurred. Adults typically have a greater need for follow-up testing, although children may require it, too. Some doctors recommend a routine re-biopsy if you are diagnosed in adulthood, as healing is often quite slow and uncertain.
It also can be helpful to follow up with an expert dietitian for assistance in adapting to, and maintaining, a healthy, nutritious, gluten-free diet.
Medications to control intestinal inflammation
If your small intestine is severely damaged, your doctor may recommend steroids to control inflammation. Steroids can ease severe signs and symptoms of celiac disease while the intestine heals.
Dermatitis herpetiformis
If you have this itchy, blistering skin rash that sometimes accompanies celiac disease, your doctor may recommend a skin medication (dapsone) along with the gluten-free diet.
Refractory celiac disease
If you have refractory celiac disease, you may continue to have severe symptoms, or your symptoms may lessen but then relapse. In either case, your small intestine does not heal. When this happens, you likely will require evaluation in a specialized center. Refractory celiac disease can be quite serious and there is currently no proven treatment.
People with refractory celiac disease should be treated by experts. There may be several causes for this condition. Doctors will often use steroid therapy either a topical budesonide or systemic steroids such as prednisone. Sometimes, they will use the same medications used to treat other conditions.
Potential future treatments
While the only proven therapy for celiac disease is a gluten-free diet, it is not perfect. People with celiac disease may often be accidentally exposed to gluten, possibly causing severe symptoms.
Several treatments are in development for celiac disease. Some try to neutralize or bind to gluten. Others address the barrier of the intestine, blocking the leakiness that gluten can trigger. Still others target the body's immune system. Researchers have also been trying to genetically modify wheat, but have not yet been successful.
None of these treatments is likely to be approved within the next two to three years. However, given the number of different approaches, there is a good chance that there will be additional treatments available for celiac disease in the future.
Clinical trials
Lifestyle and home remedies
If you've been diagnosed with celiac disease, you'll need to avoid all foods that contain gluten. Ask your doctor for a referral to a dietitian, who can help you plan a healthy gluten-free diet. It's important to get enough vitamins, nutrients, fiber and calcium in your diet.
Here's an overview of foods that contain gluten and gluten-free foods that are safe to eat.
Always avoid
Avoid food and drinks containing:
- Barley
- Bulgur
- Durum
- Farina
- Graham flour
- Malt
- Rye
- Semolina
- Spelt (a form of wheat)
- Triticale
- Wheat
Read labels
Packaged foods should be avoided unless they're labeled as gluten-free or have no gluten-containing ingredients. In addition to cereals, pastas and baked goods — such as breads, cakes, pies and cookies — other packaged foods that may contain gluten include:
- Beer
- Candies
- Gravies
- Imitation meats or seafood
- Processed luncheon meats
- Salad dressings and sauces, including soy sauce
- Self-basting poultry
- Soups
Certain grains, such as oats, can be contaminated with wheat during growing and processing. Pure oats are not harmful for most people with celiac disease. In the United States, doctors generally recommend avoiding oats unless they have been specifically labeled gluten-free. Outside of the United States, different labeling laws for oats apply. Occasionally, even pure oats can be a problem for people with celiac disease.
Allowed foods
Many basic foods are allowed in a gluten-free diet, including:
- Fresh meats, fish and poultry that aren't breaded, batter-coated or marinated
- Fruits
- Most dairy products
- Potatoes
- Vegetables
- Wine and distilled liquors, ciders and spirits
Grains and starches allowed in a gluten-free diet include:
- Amaranth
- Arrowroot
- Buckwheat
- Corn
- Cornmeal
- Gluten-free flours (rice, soy, corn, potato, bean)
- Pure corn tortillas
- Quinoa
- Rice
- Tapioca
Carob is a potential substitute for gluten, but more research is needed about its effect on people with celiac disease.
Fortunately for bread and pasta lovers with celiac disease, an increasing number of gluten-free products are available. If you can't find any at your local bakery or grocery store, check online. There are gluten-free substitutes for many gluten-containing foods. However, be aware that processed gluten-free foods may contain excessive fat and calories.
Alternative medicine
There are no proven treatments that assist with celiac disease. Enzyme therapies that claim to digest gluten may be available in health food stores or other outlets, but there is no scientific evidence that they are effective in treating celiac disease.
Coping and support
It can be difficult, and stressful, to follow a completely gluten-free diet. Here are some ways to help you cope and to feel more in control.
- Get educated. Educate those around you — including family and friends — so they can recognize, acknowledge and support your efforts in dealing with the disease.
- Follow your doctor's recommendations. If you are diagnosed with celiac disease, it's necessary to maintain a totally gluten-free diet.
- Find a support group. It's helpful to know that you're not alone. You may find comfort in sharing your experience and struggles and meeting people who face similar challenges. Organizations such as the Celiac Disease Foundation, Gluten Intolerance Group, the Celiac Support Association and Beyond Celiac can help put you in touch with others who have had similar experiences and can understand what you're going through.
Preparing for your appointment
You may be referred to a doctor who treats digestive diseases (gastroenterologist).
Here's some information to help you prepare for your appointment and know what to expect from your doctor.
What can you do
- Continue eating a normal diet. If you stop or reduce eating gluten before you're tested for celiac disease, you may change the test results.
- Write down your symptoms. Include when they started and how they may have changed over time.
- Write down key personal information. Include any major stresses or recent life changes.
- Make a list of all medications. Include vitamins or supplements that you're taking.
- Write down questions to ask your doctor.
Questions to ask your doctor
Some basic questions to ask your doctor include:
- What's the most likely cause of my symptoms?
- Is my condition temporary or long term?
- What kinds of tests do I need?
- What treatments can help?
- Are there any dietary restrictions that I need to follow?
- How will I learn which foods contain gluten? Should I see a dietitian?
- If I have celiac disease, will you also test for other conditions such as vitamin or mineral deficiencies, osteoporosis or diabetes?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Be ready to answer questions your doctor may ask:
- When did you first begin experiencing symptoms, and how severe are they?
- Have your symptoms been continuous or occasional?
- What, if anything, seems to improve your symptoms?
- What, if anything, seems to worsen your symptoms?
- What medications and pain relievers do you take?
- Does anyone in your family have celiac disease?
- Do you or does anyone in your family have an autoimmune disorder?
- Have you had any blistering or itchy skin rashes with your symptoms?
- Have you ever been diagnosed with anemia or osteoporosis?